The global markets challenge the position of the pharmaceutical human businesses with different demands, like ways of pricing, patient orientation and ESG (environment, sustainability, and governan…
Get Started for FREE
Sign up with Facebook Sign up with X
I don't have a Facebook or a X account

| Tags |
|---|
 Your new post is loading... Your new post is loading...
Digital Health, eHealth and Mobile Health, are said to be disruptive to health care. Yet, governments and payers trust it to be cost saving and quality building. What is? E-Health, Telemedicine and…
eHealth – The Introduction.. See in a short overview what ehealth actually is and what steps you may take to apply it to your proper organization. Furthermore: learn about the ehealth thought…
rob halkes's insight:
Discussions about health care reform might be supported by a clear view on eHealth and digital health. I guess this post describes it.
Overview Electronic health records have transformed modern medicine, giving doctors and nurses better data to guide care, supporting enhanced patient safety through new automated tools, and creating more efficient processes by connecting different health systems. However, the design, customization, and use of electronic health records (EHRs) by doctors, nurses, and other clinicians can also lead to inefficiencies or workflow challenges and can fail to prevent—or even contribute to—patient harm. For example, an unclear medication list could result in a clinician ordering the wrong drug for a patient. Laboratory tests that are displayed without the date nd time of te results could lead to clinical decisions based on outdated information. And failures of systems to issue alerts about harmful medication interactions—situations that can stem from changes made by facilities, how clinicians enter data, or EHR design—could lead to medical errors. These safety hazards can be associated with EHR usability, which refers to the design and use of the technology and how individuals interact with it. Usability challenges can frustrate clinicians because they make simple tasks take longer, lead to workarounds, or even contribute to patient safety concerns. These challenges can stem not only from the layout of EHRs, but also from how the technology is implemented and operated in health care facilities; how clinicians are trained to use it; and how the EHR is maintained, updated, and customized. Each stage of EHR development and use—the software life cycle from development through implementation and use in a health care environment—can affect the usability and safety of the technology. While usability and patient safety are related, not every usability challenge will represent a risk to patients, and not every risk to patients stems from an EHR usability problem. In fact, some changes to EHRs might improve safety but result in less-efficient workflows—for example, if clinicians were prompted to enter “lbs.” or “kg.” every time they entered a patient’s weight. But when a system is challenging to use or patient information is difficult for a clinician to find, safety risks could occur. As part of federal criteria that provide the certification standards for EHRs, technology developers must state that they engage end users and conduct usability testing during design and development. However, the certification requirements can fall short in two ways when it comes to assessing whether the use of products contributes to patient harm. First, current federal testing criteria do not address circumstances in which customized changes are made to an EHR as part of the implementation process or after the system goes live. Instead, current rules focus only on the design and development stage of the EHR. While federal regulations mandate the testing of certain safety-related features—such as medication-allergy checks—the requirements do not focus on whether those functions operate in a safe way. The second key challenge is the absence of requirements and guidance on how to test clinician interaction with the EHR for safety issues. Clinical test cases, which are scenarios that reflect realistic patient conditions and
To address these two challenges, The Pew Charitable Trusts, MedStar Health’s National Center for Human Factors in Healthcare, and the American Medical Association conducted a literature review and convened a multidisciplinary expert panel composed of physicians, nurses, pharmacists, EHR vendors, patients, and health information technology experts. This information led to the development of: Recommendations on how to advance usability and safety throughout the EHR software life cycle, which can be used as the foundation for a voluntary certification process for developers and EHR implementers.Criteria detailing what constitutes a rigorous safety test case and the creation of sample test case scenarios based on reported EHR safety challenges. Use of the voluntary certification tenets and test cases by health care facilities and technology developers can improve the usability and safety of EHRs. They also allow for the proactive identification of potential harm associated with the implementation and customization of EHRs See at PEW: here also for download
rob halkes's insight:
Gr8 insight by a recent survey by PEW addressing the very transfer from IT technology into actual practice of health care provision in real world and real time! Addressing possible and potential hazards in using Electronic Health Record by different people from different disciplines in health care. A must read for anyone active in healthcare with EHR's, patients inlcuded. That's why the eHealth thought lab works in three steps, planning nt only the concept of ideas to real applications, but also implementing its use to work effectively. See our eHealth elaboration here
Set goals first. If traffic, leads and sales are part of the goal, then gotta have the next focus be on content creation. Then, using social to share. Can't get much value out of social unless you're actively creating, publishing and sharing content. Via nrip
rob halkes's insight:
You might think that after 10+ years, social media for healthcare is a self evident activity,! Nothing is less true, however ;-) But here's a checklist you need if you still need to sign up ;-)
New report (May 2017) from Ericsson
Key findings
Consumers are frustrated with inconveniences and doctor wait times; 39 percent of chronic patients prefer online consultations to face-to-face meetings. Close to two in three consumers say wearables that monitor and administer medication are important to better manage chronic ailments,leading to reduced visits to the doctor. More than half of cross-industry decision makers feel decentralizing healthcare to local centers will improve efficiency and address resource scarcity.
35 percent of consumers say that online access to a central repository of medical records will help them easily manage the quality and efficiency of their care; 45 percent of cross-industry experts consider the central repository as a breakthrough in healthcare provisioning. Access to patient data is considered important to improve healthcare. Doctors will become data scientists and data security will become paramount, as 46 percent of cross-industry decision makers already consider data security to be an issue.
56 percent of consumers worry about their wearable health patches running out of battery; 42 percent of cross-industry decision makers expect devices connected to 5G networks to consume less power. 61 percent of consumers say remote robotic surgery is risky as it relies on the internet; and 35 percent of cross-industry decision makers expect 5G to provide reliable low-latency connections. 47 percent of telecom decision makers say that secure access to an online central repository is a key challenge and expect 5G to address this.
rob halkes's insight:
Mobile development in health care provision demands integrated care. We 've said it before: it urges all stakeholders to work together in a co-creative way - not just "doing things with each other" See http://bit.ly/co-creation-in-care ). There's more to designing care than just settling on who does what. The art of doing business in care is a thing to learn. There are three different kinds of care: See http://bit.ly/Integration-of-care
In an opinion piece published online in Medical Economics, part of the Modern Medicine Network, Henry Anhalt, DO discusses the current status of Precision Medicine as 2016 draws to a close. Reflecting on President Obama’s 2015 State of the Union address, in which he launched the Precision Medicine initiative – a program that aims to revolutionize health outcomes by taking a personalized approach to medicine and research – he acknowledges the ongoing debate as to whether this approach to treating disease can truly deliver on its promises. He also recognizes the uncertainty for precision medicine that lies ahead as the US enters a new presidential term.
rob halkes's insight:
Well established and short opinion on Precision medicine. Good to see the new journal too! Let's hope that this Obama initiative survives Trump's presidency! Why don't you share this to state your point?
Population health strategies have the benefit of advanced remote monitoring and telemedicine capabilities than in decades past, but to create a truly successful telehealth program you have to keep an open mind. That is the message that Banner Health, an integrated, nonprofit health system based in Phoenix, Arizona, has taken to heart from its ongoing ambulatory care program for patients with chronic and complex diseases which is powered by Philip’s telemedicine platform. [...] The program – named Intensive Ambulatory Care or Banner iCare — launched June 1, 2014, and the goal was to provide better care and reduce costs for the most complex patients – those with two or more chronic conditions — who happen to account for the highest cost in terms of healthcare dollars spent on their care. Many population health programs focus on one chronic disease or another, but Dr. Hargobind Khurana, senior medical director of health management at Banner Health, said Banner’s approach was different. “The idea was to say that there are complex, chronic patients who don’t have one chronic disease but have multiple chronic diseases and they have a hard time managing these diseases …these patients keep coming to the ED. They are in and out of the hospital,” he said in a recent interview. “Our goal was to be more broad than just one or two chronic diseases, so we focused on this aspect and said let’s find the high-utilizers who end up [repeatedly] in the hospital, in the ED.” [...] But the population health strategy isn’t just high-tech. It is high-touch too. “There’s a large team central team that’s dedicated for this work – health coaches that go to the patient’s home, there’s a social worker, there’s a pharmacist there are tele-nurses and there’s a physician who kind of helps coordinate their care,” Khurana explained.[...] When the program launched, not enough patients who Banner felt could benefit were choosing to participate. The reason was simple: they didn’t want to switch their primary care providers as the program protocol required. “We went in with this program thinking that what we would do is we would identify these patients and we’ll become their entire care team, so basically we would go to these patients and say, ‘We will become your primary care physician and we would also be the care team that would help with the telehealth platform,'” Khurana said. “Part of the lesson learned there was that patients were hesitant in the idea of leaving their PCP and entering a new entity.” So Banner iCare pivoted. “So we changed that model about a year into it and told them, ‘You don’t have to leave your PCP. We will be an add-on to your care team. So you will have your PCP and you will work with them but we will be supporting your care as an addition to your PCP,’ ” he recalled. “That really helped the patients feel more comfortable joining my team, andI think that was a good learning.” Changing the model based on feedback shows that in year two Banner Health was willing to take on the additional complication of keeping PCP’s apprised of any intervention they did to help the PCP’s patients. All without overwhelming the primary care doctor with raw data that was being transmitted through Philips’ telehealth platform. Currently, about 500 patients are being cared for using the Banner iCare program and to date more than 1,000 have utilized the program. Khurana said people drop off when they move, change health plans, or die, adding that very few people leave the program because they didn’t like it. Banner has seen some savings too. The Banner iCare program has reduced the total cost of care per beneficiary by 27% per year. It has also reduced hospitalizations by 45%. The program is ongoing, and Khurana believes that while they have hit upon an effective program, all the answers aren’t available yet. For Philips, which codeveloped the program with Banner, there have been some important lessons too. “We learned and showed that telehealth technologies can have a big impact on the care for patients dealing with multiple chronic conditions,” said Jeroen Tas, CEO of Philips Connected Care and Informatics, in an email. “We also learned that the process of integrating telehealth and other connected health solutions is a delicate one. It will only be successful if existing care pathways are redesigned. Change management and education are needed too as telehealth enables a more integrated and multidisciplinary care team approach than the traditional doctor-patient interaction.” That traditional assumptions must be questioned was something that Banner Health also learned through the iCare program. And those assumptions center around who is a high-cost patient.[..] “You can’t use retrospective costs or utilization data and assume that it would be the same in the future because it doesn’t account for the regression to the mean,” Khurana said, adding that just because some patients “had a bad year doesn’t mean that they are going to keep having bad years, year after year after year.” In other words, the entire thinking about who is going to be an expensive patient in the future requiring coordinated care needs to be overhauled. “We have to be smarter in building and developing more intelligent algorithms to identify patients who would be future high utilizers,” he said. “That will be the next focus of population health – to have better predictive analytics.”
rob halkes's insight:
Banner Health learned old assumptions must be put aside to develop a patient-centered telehealth program by harnessing home monitoring devices, tablets for video consults, all integrated and powered on Philips Healthcare's software. Experience teaches that telemedicine and ehealth is an all encompassing effort: patient trust, medtech, mobile applications, but also the healthcare providers team must be adequately designed in order to gain trust AND to be effective. Design and development for implementation is as crucial as working tech and multidisciplinary coordination.
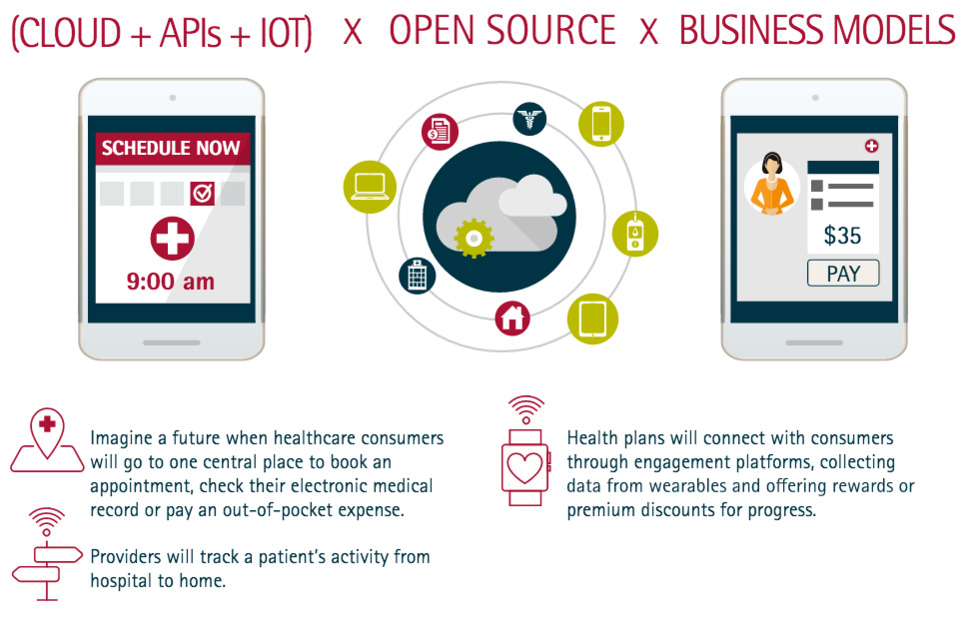
Ecosystems are the new bedrock of digital healthcare. Platforms are enabling smart cities, connected machines, robust customer analytics and more. In healthcare, they provide the underlying technology that can make healthcare experiences more connected. Some companies have taken the plunge into platforms, while others are just beginning to use digital technologies and cloud foundations as a first step into the platform world. Platform potential The power of platforms should not be underestimated. More than ever before, they can link the entire healthcare ecosystem—from patients to providers to health plans. Imagine a future when healthcare consumers will go to one central place to book an appointment, check their electronic medical record or pay an out-of-pocket expense. Providers will track a patient’s activity from hospital to home. Upon discharge, data from a patient’s blood pressure monitor, coupled with analytics, could indicate a pending complication and give providers ample time to take corrective action. Health plans will use platforms to connect with consumers in more meaningful ways. For example, some are using engagement platforms, such as Rally Health and Welltok, to collect data from wearables and give rewards or premium discounts for progress. Platform privileges Platforms can help reduce out-of-pocket costs by supporting healthier lifestyles among consumers. Furthermore, they make previously difficult to access services more mainstream. Take for instance leading health plans that are making wellness programs available to the masses because platforms make it easy and cost-effective to scale such offerings and integrate into existing experiences.
rob halkes's insight:
From disrupted care to #ehealth #integratedcare #iot and #platforms: see the strategic roadmap for health as imagined by Accenture: a scenario to think about! #pharma are you "in" ?
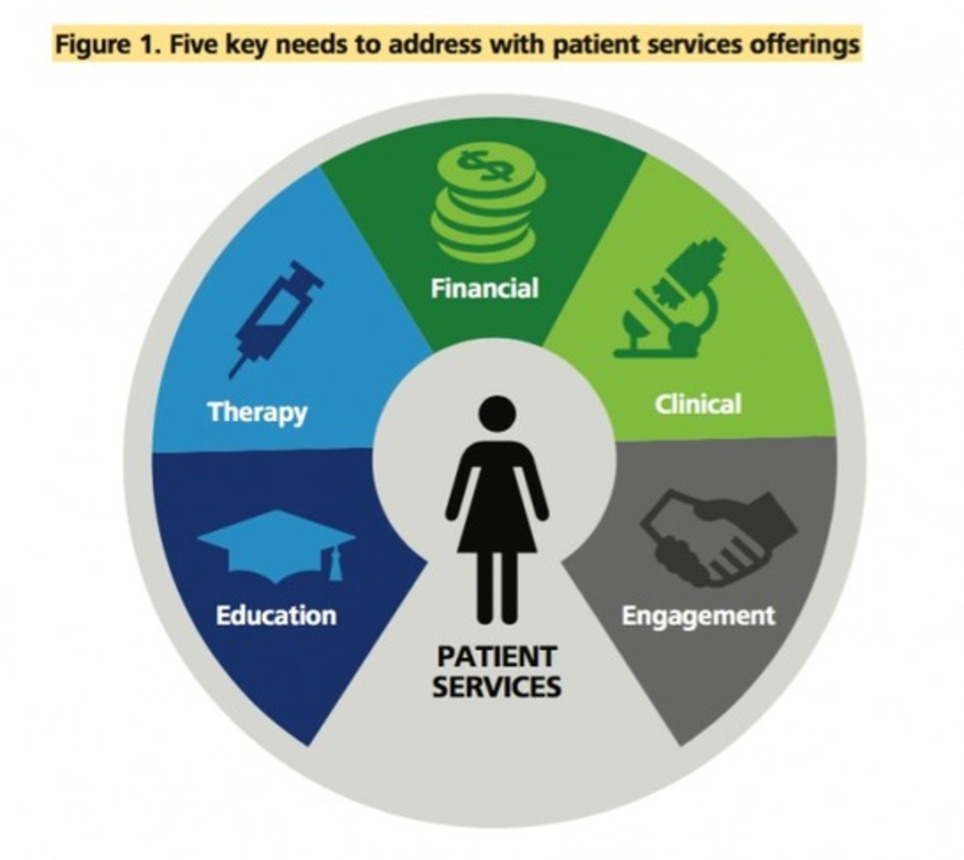
Patients are demanding care and solutions that are coordinated, convenient, customized, and accessible, and a number of nontraditional health companies are coming forward to address these emerging expectations, even as many large pharmaceutical companies focused on traditional markets have lagged behind. Life sciences companies have a window of time to frame their patient engagement strategies (Deloitte Review, 2016,18) for operating in the new, customer-centered, digital ecosystem— or risk the new players keeping them constrained within the traditional pharma model. [...] The explosion of research in the area of patient engagement further speaks to the need for timeliness on the part of pharmaceutical companies implementing and executing engagement strategies, and nonprofit and public sector organizations can play a key role in making this happen. [...] It makes sense that pharmaceutical companies would look to establish their brand for patient engagement services. Being able to deliver consistent service to patients and health care providers alike is paramount in building trust and loyalty. Conversely, and unsurprisingly, poor execution can drive the optics of a company’s brand in the wrong direction. With regard to patient engagement, there is emerging support for moving away from a reactive approach, in which coordination between stakeholders, therapy, and care is limited or ad hoc, to a proactive model in which engagement tools and support bolster both patients and health care providers. Over the last three to five years, we have observed life sciences companies beginning to implement cloud-based platforms on which internal and external users can access the same platform, allowing the company to centrally control data access, ensure data quality, easily generate real-time reports, and quickly distribute system updates to all users. [...] This report is great and pharma organizations should be aligning their organizations to increase patient engagement and think of new ways to reach and interact with patients. This means striving to continually improve engagement through a patient centered approach at a time when a lot of people are going to have a hard time justifying the ROI. Read on here: http://bit.ly/1TSpvQD
rob halkes's insight:
Great review of Deloitte's study on patient engagement strategies! Several aspects about its necessities are given, resp. discussed:
However, pharma companies need to learn first how to engage themselves with patients and more specifically patient advocacy groups. Look here at PatientView about what patients' perceptions of the reputation of pharma companies is and for further information as to how you as a pharma company can increase your company's competency to align, service and work with patient groups: http://bit.ly/PatientView
Consumers want technology to monitor every aspect of their life and Wearable Tech, IoT and all emerging technologies are working together towards such goal. The question remains: Will this help or hurt providers’ efforts?
rob halkes's insight:
Technology itself creates expectations. Handling these and making them true is a challenge. Lots of healthcare providers are relucatant to their impact. eHealth thinking and realization can go in manageable steps creating your proper roadmap. See here
About the Precision Medicine Initiative
Far too many diseases do not have a proven means of prevention or effective treatments. We must gain better insights into the biology of these diseases to make a difference for the millions of Americans who suffer from them. Precision medicine is an emerging approach for disease treatment and prevention that takes into account individual variability in genes, environment, and lifestyle for each person. While significant advances in precision medicine have been made for select cancers, the practice is not currently in use for most diseases. Many efforts are underway to help make precision medicine the norm rather than the exception. To accelerate the pace, President Obama unveiled the Precision Medicine Initiative (PMI) — a bold new enterprise to revolutionize medicine and generate the scientific evidence needed to move the concept of precision medicine into every day clinical practice. Read about the scientific justification of the Precision Medicine Initiative in a New England Journal of Medicine Perspective by NIH Director Dr. Francis S. Collins and former NCI director Dr. Harold Varmus.
rob halkes's insight:
Who could be against it? "Precision Medicine": The next logical step to eHealth: integrate personal data and biophysical parameters and adapt the treatment to a person.. Something we always intended too, didn't we?
Most doctors in France, Germany and the UK believe innovations such as wellness apps and wearable monitors are here to stay. However, they also see some drawbacks. See this blog by eMarketeer based on research by Ipsos Healthcare Doctors throughout Europe already work in an environment full of advanced technology, including highly sophisticated diagnostic and surgical equipment and other state-of-the-art devices. These days, though, they also need to deal with the gadgets in the hands of consumers—their patients. And doctors have mixed feelings about the explosion of mobile apps, wearables and other digital tools aimed at boosting consumers’ awareness and control of their own health. That’s not to say that medics don’t see essential value in a lot of the new tools on offer. According to the “Digital Doctor Report 2015” from Ipsos Healthcare, 72% of doctors polled in France, Germany and the UK had either used or recommended an app, online health forum or wearable technology in the previous year. While four in every five doctors felt technology was increasingly important and would play a permanent role in healthcare, many were unsure what that role would be. For example, most doctors sampled by Ipsos were wary of overstating the benefits of mobile health apps. Some 13% said that mobile technology would eventually replace routine checkups for stable patients with chronic problems—but 26% disagreed. One in 10 said that disease/compliance monitoring apps used alongside drugs would become a prerequisite for patients being reimbursed by insurance companies for their health expenses—but 37% said this wouldn’t happen. Asked whether apps were key to improving patients’ adherence to health regimes, 15% of doctors said they agreed—but 21% said apps were not key. Moreover, significant numbers of doctors had doubts about the usefulness of some digital health solutions, at least in their current form. Mobile technology such as apps and wearables were a particular focus of concern—though the level of worry varied from one country to another. In the UK, for example, the overwhelming majority of the sample agreed that “mobile technology is a reliable means of monitoring health data”; just 11% disagreed. But in France, 24% disagreed, and in Germany, the proportion was 29%. Similarly, most doctors did think mobile technology would help simplify access to healthcare. But more than one in 10 in the UK and Germany did not agree. In France, a notable 33% of doctors did not subscribe to this view. Many doctors in the Ipsos study were also thinking ahead to potential conflicts arising from consumer use of apps and other digital tools. After all, most healthcare professionals in advanced economies have already seen large numbers of patients self-diagnosing with the aid of Google search or the websites of medical organizations—and arguing with their doctors as a result. While doctors polled by Ipsos generally acknowledged that technology could help with therapy and monitoring chronic conditions such as diabetes and heart ailments, 27% feared that mobile apps would create more conflict with patients. Again, the top worries varied by country. Nearly two-thirds of doctors in the UK were concerned that patients could misinterpret data from digital health tools. In Germany, about six in 10 respondents felt these tools could fuel hypochondria, and in France, more than half of doctors were unhappy about the lack of security and privacy involved in using them. Because the application of digital technology to day-to-day consumer healthcare is pretty new, most doctors (73%) couldn’t say exactly what they wanted it to do. But among those that did have a clear view on this, monitoring was the top function they identified. See more at: http://www.emarketer.com/Article/Europes-Doctors-Embrace-Digital-HelpersUp-Point/1012837?ecid=NL1002#sthash.bqTvbQbq.dpuf
rob halkes's insight:
Inspiring information on Doctors' views on ehealth! Do they represent doctors' beliefs in digital apps? Are they cautious about negative impact on therapy, diagnosis? Don't they trust their patients with digital? Or be it all concerns about the sustainability of their medical business, fear for fundamental change? Who would say? I guess further research!
Blogs, Journals, News, White Papers To help small practices, vendors need to think like patients
A report on a series of presentations on patient engagement at HIMSS15. The presentations included statistics on patients strong preferences to be notified by texting of appointments and other reminders and their desire to be equal partners in healthcare decision making Telemedicine market to soar past $30B Why what works for Uber may not work for medical apps While many innovators and futurist like to see Silicon Valley startups with high valuations as a model for healthcare. This excellent piece points out the weakness of this argument - healthcare is based on a social contract, the risk of losing everything (not an option in healthcare), unnecessarily galvanizing the opposition, misreading the law, Uber’s strategy hasn’t even worked in the transportation industry yet (they now have 70 lawyers). Patients and Families as Partners Amer Haider of the startup Doctella shares his experience with his father’s hospitalization and the frustration of trying to obtain personal health information. Amer is an advocate of involving patients in patient safety through the use of checklist, but this hospital frustrated his attempts to get involved in a family member’s care. My Medical Records | How To Get Them From the Louisiana Health Quality Forum which is promoting getting one's health data - how and what to get - directly to patients. An important direct to consumer approach which should be copied by other states. This strong argument for patient access to medical records proposes an approach from a Frost and Sullivan white paper on using PHIEs rather than HIEs to get patients their data. Quotes leaders in the field including David Kibbe.. Sharing Your Fitness Tracker Data? ‘Pace’ Yourself This article discusses the potential uses of fitness tracking devices in research. Runkeeper meets researcher. Social Media Use in Chronic Disease: A Systematic Review and Novel Taxonomy From the American Journal of Medicine, this literature review showed that "48% of studies indicating benefit, 45% neutral or undefined, and 7% suggesting harm. Using social media to provide social, emotional, or experiential support in chronic disease, especially with Facebook and blogs, appears most likely to improve patient care." 5 Things You Should Know About Your Electronic Medical Records From the Cleveland Clinic blog, a good basic primer for patients on their portal. The author, Steven Nissen, MD, warns that it may include medical jargon you may not understand but it will keep you well informed about your health numbers and your doctor's recommendations (assuming your portal has Open Notes). The 2015 #HIT99 Results Are In.. .
rob halkes's insight:
Very inspiring collection of presentations and outcomes of the HIMSS meeting! Every bit a stimulating read. Each a fundamental aspect of getting to ehealth 
Lionel Reichardt / le Pharmageek's curator insight,
August 10, 2015 6:03 AM
Very inspiring collection of presentations and outcomes of the HIMSS meeting! Every bit a stimulating read. Each a fundamental aspect of getting to ehealth 
SergePPlourde's curator insight,
August 10, 2015 9:47 PM
Very inspiring collection of presentations and outcomes of the HIMSS meeting! Every bit a stimulating read. Each a fundamental aspect of getting to ehealth
"Portal me" ... It is the way we finally want to go: integrated hard and software all directed at a healthier life in cooperation with professionals, insitutes, family, friends and peers we do want... Jeff Belden inspires!
rob halkes's insight:
Jeff Belden message may inspire lots of health care professionals, authorities and others to more activity towards development of ehealth applications. It doesn't need to be through a all in once leap, but a step by step process may benefit all stakeholders! See him motivate!
eHealth - The Introduction..
rob halkes's insight:
A precis about ehealth = Learn how you could direct your way to ehealth initiatives and the direction into your future of provision of care
Amsterdam, the Netherlands – Royal Philips (NYSE: PHG, AEX: PHIA) and Leiden University Medical Center (LUMC) today announced a new research collaboration aimed at improving preventative care and chronic care through wearable technologies. The organizations intend to attain new data-driven insights into the relationship between lifestyle and health in elderly people. This will support the development of personalized coaching solutions using wearable sensors to help people to age more healthy and reduce the impact of illness and chronic conditions.
As people live longer and lifestyles change, more people are confronted with chronic disease. In addition to having a major impact on people’s quality of life, this puts increased pressure on healthcare systems.
New wearable sensor technologies are rapidly becoming available and could play an important role in healthy lifestyles and treatment compliance. The current challenge is to turn the data these new devices offer into clinically relevant information. This will help build scientifically proven and clinically validated solutions to improve the outcomes of lifestyle intervention programs and medical treatments.
See more here
rob halkes's insight:
We know by now of the potential of digital applications in health, mhealth and wearables. But we need these intitiatives like Philips and LUMC announced today to gain insights whether it works, bbut also how it works and how it might me implemented in real care. Congrats!
Implementing an eHealth initiative is the first step in moving your healthcare organization to the forefront of eHealth technology. For instance, how would your organization make use of this revolutionary eHealth initiative innovation? How would you react if patients began asking to connect their eHealth applications to your information system? eHealth initiatives require an analysis of your entire workflow from operations to systems and technology, from clinical and financial performance to implementation. eHealth initiative general outcomes expected include benefits to providers and to patients, rapidly expanding technological tools, and even more use of internet based activities. Working with The Fox Group’s eHealth experts through our three strategic eHealth Thought Lab meetings allows you to get customized knowledge on the processes and strategic changes that must be made in order to maximize the eHealth initiative potential within your organization. Each eHealth Thought Lab meeting will be tailored to your situation, and can jump-start your organization’s eHealth initiatives. By the end of this series of three strategic meetings, you will have an appreciation of the potential for your organization to embark on a meaningful eHealth initiative. [..] I. The Current eHealth Initiative: a short, to the point workshop introducing the main elements of the eHealth initiative, a working definition, the effectiveness and implications of eHealth in the future. You select the proper internal stakeholder audience of your organization.
II. eHealth Discussion and Analysis: a workshop reviewing your current eHealth applications, including electronic health record systems, mobile health, internet-based, social media interaction tools, telemedicine, and similar components. It will also address your organizational enthusiasm and/or challenges to creating a strategic planning process addressing the future in eHealth technologies as they unfold. Discussion between your representatives and experts from The Fox Group will run deep into several aspects of the eHealth initiative phenomenon.
III. eHealth Strategic Planning: a strategic workshop, where you discuss currently existing concepts, modules, and devices available to you and your patients. The final step is to identify the strategic actionable steps to implement your eHealth initiative, bridging the gap between what is available and what needs to be developed.
rob halkes's insight:
This is my and the Fox group's take on approaching ehealth. Yes it is promotional, but firmly based on experience and expertise. I thought one could do with the three step approach: update on what, discussing the impact for you and setting up a clear and effective plan to accomodate and develop your practice in health
rob halkes's insight:
Great Insights from patients' themselves baout their experiences as unmet needs in usoing their health apps!
The Dutch ehealth monitor of the Netherlands has been released recently. There is no English translation yet, nor a summary, but a English infographic is presented at this post on the website. Here you can see that ehealth is steadily but I guess, firmly growing in NL. More healthcare users say their GP allows them to make online appointments: from 7% in 2013 to 13% in 2014; or request repeart prescriptions: from 21% to 30%. More GP's, 93% to 98% (!) and medical specialists, 66% to 75% use mainly or exclusively electronic records! However no major shifts are found in the use of eHealth compared to 2013. There will be greater coordination in the area of eHealth. The Ministry of Health Welfare and Sport sets concrete objectives, and parties 'in the field' seek each other out for joint activities! Four things stood out in the study:
For a real, large scale use of eHealth a good balance is needed between the investment in money and effort and the experience added value in terms of imprived care, convenience and financial benefits. See here for Nictiz and here for Nivel the sources and down;oads of inforgroaphic (in English too) and the report (Dutch).
rob halkes's insight:
I would say that experience demonstrates that ehealth initiatives may be initiated by small efforts to digital services from physicians to patients, like repeat prescriptions. These are relatively easy first steps. I reckoned that on the basis of my own experience from early on. See some information to this here.
Telemonitoring reduces readmissions 44 percent in 4-year, 500-patient study | mobihealthnews #hcsmeu
rob halkes's insight:
Research on eHealth now presents data that it really can safe costs. Not "just like that" of course, but one needs to accommodate to get to these results. See for instance here, to things to be thought through: http://www.healthbusinessconsult.com/telemedicine-ehealth-mobile-health/

Michael Seres's curator insight,
November 22, 2014 8:16 AM
Will that percentage increase with the growth of #wearables
From Rob Halkes, manager Patient View in the Netherlands, and advisor to Health20. This uear's edition of Health20, London, November 10-12, will especially be of large interests to both Health App developers, Healthcare providers and patients. Alexandra Wyke from PAtient View will present the outcomes of the first global research for Patients' wishes and demands regarding their health apps. Here is a first view to the outcomes, But at the conference more will be presented!
rob halkes's insight:
I am very thrilled to view the scoop presentation by dr. Alexandra Wyke on the first day of Health20 in London2014, November 10th: "Choosing and Prescribing an App!" - based on the first global research of patients' wishes and demands about their Health Apps. Do you wan to come, make your reservation with this 15% reduction code: SPCL15 ! You're welcome!
{…] The title of my talk was “Giving Up Control: Leading in the Digital Era”. One key data point from Gallup that continues to astound me is that worldwide only 13% of people are engaged in their work. It’s higher in the US, standing at 30% but that’s still terrible! I believe that a big reason for this is that we don’t give enough autonomy to, and respect the growing agency of our employees, especially for the Millennials who crave purpose and meaning in their work. The hierarchies that exist in our organizations were designed for a bygone era where efficiency and scale were paramount. But today, speed, innovation, and creativity are the sources of competitive advantage. Companies have been responding, deploying collaboration platforms and enterprise social networks to connect people throughout the organization. Shrinking the distance between previously siloed departments, or between executives and the front lines sounds great — unless you’re a middle manager. The biggest problem leaders face in the digital era is that power and influence are being decoupled from titles and organizational structure. So how can you be an effective leader? Here are the three things that organizations can do:
What each of these has in common is the need to give up control. In the talk, I shared the journey I’m going through as the parent of teenagers, as they push for greater autonomy and trust to make their own decisions. In our work, if we truly want to have an engaged workforce, then we’re going to have to lead differently, and establish a new kind of relationship and trust that’s created and deepened with these digital tools.
rob halkes's insight:
Working within the health care market I do witness daily the struglle of employers and employees, both within organizations of health care providers and of the industry to respons in a meaningful way to digital "disruption". Digital disruption has its potential to turn upside down every routine one uses tot get the job done, to approach customers/clients and to create value to business How to respond to forces that do have this 'threat'? Charlene discusses the leadership role. It goes further than that, but this is crucial. When leadership cannot acommodate, how sould the rest of the organization cope? This is certainly true for much of the pharma and devices companies, where leaders tend to hold on to market approaches that were successful in the days gone by. They should orientate themselves to new possibilities of customer approaches, not as an add on to what was done before, but to a new integrated system of engagement. Believe me, I could tell!
Most accountable care organizations have health information technology in place to improve quality and lower costs, but many say difficulties with data exchange are keeping them from reaching their potential. Of the 62 ACOs polled by Premier healthcare alliance this past summer, 88 percent report "significant obstacles" in integrating data from disparate sources. Also, 83 percent say they have a hard time fitting analytics tools into their workflow. As ACOs grow, gathering data from more and different care settings, these challenges become more accute, according to Premier. Cost and ROI are also cited as key roadblocks to more effective implementation of health IT, according to 90 percent of respondents. Even when ACOs have successfully merged health IT systems, "they aren't able to effectively leverage data and analytics to derive value out of their investments given the pervasive issues with data quality, liquidity and access, as well as issues with integrating data from disparate sources," said Keith J. Figlioli, Premier's senior vice president of healthcare informatics, in a press statement announcing the findings. The numbers reported in the survey suggest interoperability is a "pervasive problem among ACOs, and it could stymie the long-term vision for ACO cost and quality improvement if not addressed," Figlioli added. The good news is that ACOs are reporting heartening improvements in clinical quality (66 percent), preventive screenings and vaccinations (63 percent), chronic disease management (59 percent) and health outcomes (55 percent). But those percentages could be even higher. "While accountable care organizations are providing quality care for many patients, even more could be accomplished if interoperability issues were addressed," said Jennifer Covich Bordenick, chief executive officer, eHealth Initiative. "However, the cost of interoperability can be prohibitive for many organizations." In a Sept. 24 call discussing the report's findings, Bryan Bowles, Premier's vice president for population health solution management, noted that this new era of shifting risk from payers to providers requires a lot of these organizations, necessitating that they manage health at both an indvidual and population level, and make smart use of clinical, claims, financial and administrative data. See more here in the original blog
rob halkes's insight:
A great example showing that there's more to ehealth than just technology. Apart from this, taking ehealth initiatives, means a good think through of all aspects of the health care process. But we are getting there. Let people with experience help!
From
ctel
Representatives Diane Black (R-TN) and Peter Welch (D-VT) introduced bipartisan legislation in the U.S. House of Representatives to build upon the progress of Accountable Care Organizations (ACOs) in shifting the reimbursement of healthcare providers away from the traditional “fee for service” model to a focus on improving the health outcomes of patients. The ACO Improvement Act (H.R. 5558) will improve the ACO model by providing additional incentives focused on health outcomes, increasing collaboration between patients and doctors, and providing ACOs with additional tools, according to a news release issued from their offices. According to an article in Med City News, the legislation would allow ACOs to utilize remote patient monitoring tools and maintain and share technology that delivers images with more remote providers. Many current restrictions that apply to originating care sites would be waived for telemedicine provided through ACOs, according to the bill. “As a nurse of over forty years, I know firsthand the challenges facing health care professionals as they seek to provide their patients with the best care possible,” said Congressman Black. “It is unfortunate that the current fee for service payment system does little to encourage and incentivize providers and patients to use the most appropriate and effective health care options. By incentivizing providers to focus on improving health care outcomes instead of increasing the quantity of services provided, this legislation will help improve care coordination, increase efficiency, and mostly importantly, ensure the patient receives the best care possible.” “If we are going to reduce health care costs and increase quality, the incentives built into the provider payment system need to be changed. In short, we need to reward value, not volume,” said Rep. Welch. “Paying health care providers based on improvements in patient health rather than the number of procedures they perform is the way of the future. Our legislation will advance these payment reforms and is based on the experience of ACOs in Vermont and around the country.” Rep. Black is a member of the House Ways and Means Committee and Rep. Welch is a member of the House Energy and Commerce Committee. These two committees are the primary House committees that consider healthcare-related legislation |