Injury specialist, Dr. Alexander Jimenez reviews the middle and forefoot anatomy -- also discusses several common athletic injuries.
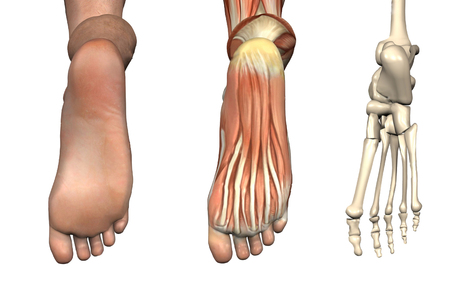
The foot consists of 26 interconnecting bones. The intricate anatomy of the foot makes it to be both a passive service structure and an active vehicle for force production (see Figure 1).
The mid foot begins at the transverse tarsal, or midtarsal, combined. The talus, navicular, calcaneus, and cuboid bones include this joint. The connections between these bones form an 'S'-shaped single joint line across the waist of the foot, with the navicular bone itself function as the structural link between the forefoot and hindfoot. The multiple articulations within the joint permit the forefoot to move independently in response to hindfoot movement. All five rays, comprised of the metatarsals and phalanges, work in concert to maximize foot stability.
Navicular Stress Fracture
A once obscure identification, navicular stress fractures, now account for 14% to 35 percent of all reported stress fractures(1). It's a particularly widespread investigation in runners, and athletes that execute volatile jumping, as in track and field sports. Suspect a navicular stress fracture in an athlete that complains of obscure mid foot pain but who can not remember actually hurting his foot. Palpation of the apex of the dorsal aspect of the navicular, called the 'N' place, causes pain in 81 percent of patients having a stress fracture(1).
The navicular lies at the crossroads of their longitudinal and transverse arches, and thus endures a unique utter stress in the middle third of the bone, where it's the most susceptible to fracture. The center third of the navicular is also the area with the least amount of vascularization. For this reason, fracture in this website resolves slowly. Treatment requires at least fourteen days in a non-weight posture throw(1).
One to 2 weeks following boot elimination, begin running and sport-specific training as tolerated, with weekly clinical evaluation of the navicular. If tenderness over the palpated navicular yields, refer for further immobilization or surgery. With conservative therapy, athletes typically return to game in five to six months, compared to three to four weeks for people who undergo surgical fixation(1).
Lisfranc Joint Injury
Named after Napoleon's field surgeon Jacques Lisfranc, who first observed this mid foot injury in men who had dropped from their horse in battle, this injury is due to forced plantar flexion at the joint. In today's sports, the mechanism of trauma is an axial load put on the elevated heel, usually from a fall or tackle by a different player (see Figure 2). Lisfranc injury is not uncommon in American football players (especially lineman in blocking stance, up on feet), football players, bicyclists, surfers, and equestrians. In sports which require feet in straps or clips, a Lisfranc injury may result in the entrapped forefoot in a fall.
An injury to the Lisfranc joints most commonly occurs medially, with a consequent separation of the first and second metatarsals, along with a dorsal displacement of the second metatarsal on the next cuneiform. Trainers with a Lisfranc injury normally present with significant pain, moderate to severe swelling, and bruising at the mid foot. Initial radiographic studies don't detect joint diastasis in up to a third of cases; therefore, weight bearing x-rays are justified if Lisfranc injury is suspected(2). An uncommon harm to the lateral Lisfranc joints happens as result of forced supination, and usually with no dislocation of the fracture or joints.
When just the ligaments of the joint are injured, care for the sprain conservatively. Begin weight bearing as tolerated but protect the joint by hammering the foot, using an orthotic shoe insert, or, in severe circumstances, immobilizing the joint using a walking fracture boot. Advance the athlete to cross- training activities, like swimming or biking, as soon as possible to keep fitness. Progress rehab to shut chain activities as tolerated. The athlete might need to utilize joint protection through taping, a shoe insert, or a stiff- soled shoe for up to 12 months(3). If the injury does not significantly improve after several weeks, ask repeated x-ray assessment in a weight bearing position.
Post-operatively, the athlete is generally non-weight posture for three to six weeks; however, encourage range of motion exercises with the feet, even while immobilized from the post-operative splint. Screw removal takes place between three to four months post-procedure, depending upon individual protocols. Rehabilitate with speed, strength, and endurance training as well as tolerated. Return to play just when the athlete illustrates closed-chain plantar flexion strength and single limb equilibrium appropriate for their sport, normally within four to six months.
Metatarsal Stress Fracture
During extended periods of training, muscles on the bottom of the foot fatigue and fail to protect the metatarsals from floor reaction forces. With no plantar muscles to dissipate this stress, the bones suffer recurrent micro-trauma that results in stress fractures.
Athletes complain of obscure forefoot pain that resolves with rest, but intensifies with continued instruction. The forefoot might be bloated and bruised. X-rays performed shortly after symptoms begin may not demonstrate a fracture; however, a bone scan or magnetic resonance image (MRI) often reveals the severe injury.
These fractures usually respond well to conservative therapy with weight bearing as tolerated but restricted activity for four to six weeks. Following six weeks, restart game training as tolerated and track for a return of symptoms. Using custom orthotics corrects biomechanical problems, such as flat feet, which could induce the athlete to repeated injury.
Dancer's Fracture
An avulsion fracture at the tuberosity at the base of the fifth metatarsal may be known as a 'dancer's fracture'. Within an avulsion fracture, the athlete complains of pain, bruising, and swelling in the base of the fifth metatarsal. This injury often accompanies a foot sprain.
Simple avulsion fractures respond well to conservative treatment of rest, ice, compression and protection. Permit weight bearing as tolerated at a splint or walking boot. Symptoms usually improve within six to eight months, at which time progressive return to sport training begins. Monitor the athlete clinically for any signs of mal-union of the fracture. Avulsions with displacement are treated surgically.
Jones Fracture
Acute fractures of the shaft of the fifth metatarsal are known as Jones fractures, called after Sir Robert Jones who first described this fracture in his own foot in 1902(4). Jones fractures happen if the heel is off of the floor and also a force is applied to the forefoot in the lateral direction, causing the ankle to reverse and roll cartilage. This region is minimally vascularized and are also the website of repetitive micro-trauma. This sort of fracture happens in amateurs, footballers, baseball and hockey players, who commonly pivot to a plantar flexed foot.
An athlete with a Jones fracture poses with pain, swelling, and bruising at the bottom of the fifth metatarsal. Weight bearing may be difficult. Fractures are categorized into three kinds. Type I is a serious fracture with clean margins and no displacement, and responds well to conservative therapy. Because of the decreased blood supply to that area of the bone, recovery takes at least six to eight months, and upward of 20 weeks to get complete calcification.
A fracture with delayed recovery is classified as a Type II. The fracture line is widened and X-ray reveals increased bone reabsorption at the margins of the fracture. A Form III is absolute non-union of the fracture. Types II and III may be because of repetitive micro trauma at the website prior to a serious event, or even the lack of vascularization which delays recovery from a serious injury. Post- surgical protocols differ, but most progress to partial weight bearing in a walking boot in one or two weeks. Athletes may start partial weight bearing activities, such as aquatic biking and training, at about fourteen days post-op and start working with shoe alterations or orthotics at six to eight weeks after surgery. Most return to sport by 12 weeks post-op.
Sesamoid Injury
The sesamoid bones are two oval-shaped bones inserted in the flexor hallucis brevis tendon, at the distal end of the first metatarsal. These bones function to lengthen the first metatarsal and assist with weight change and toe off through gait. As such, they suffer great stress in athletes that repeatedly 'push off' with the ankle in plantar flexion and the forefoot dorsiflexed, such as runners, dancers, football lineman, and golfers.
Of all sesamoid accidents, stress fracture happens 40 percent of the time, whilst sesamoiditis and acute fracture appear in just 30 percent and 10% of cases, respectively(5). As with other repetitive stress injuries, the onset of pain using a stress fracture could be insidious and vague. Passively bending the big toe can reproduce the pain. X-ray evaluation isn't always conclusive in such harms; therefore, a bone scan or MRI may be necessary for diagnosis.
Treatment consists of rest from the offending activity together with custom orthotics or a metatarsal pad to eliminate weight bearing directly to the bones. For athletes using sesamoiditis, an inflammatory condition caused by repeated stress to the bones, treat with rest, ice hockey and protection, and gradually initiate a return to action once they bear weight without pain. For those who have actual fracture, six months of non-weight bearing is necessary. If the fracture does not heal adequately following this time, consult with surgery. Athletes possibly return to sport within six months after surgery, which either partly or entirely eliminates the bone, or even fixes the fracture.
'Turf Toe'
Dancers, football lineman, rugby players, golfers, and wrestlers often assume a position of MTP joint dorsiflexion with ankle plantar flexion (see Figure 3). More and more flexible shoes, along with artificial turf surfaces, have been implicated in the greater incidence of this harm.
Participants present following an acute event with pain and tenderness over the joint, accompanied by swelling and bruising when the injury is categorized as Grades II (partial tear of the ligaments) or III. Conservative therapy with immobilization of the MTP joint through taping or bracing; protection with steel shoe inserts; progressive weight bearing; and restricted activity is the normal treatment course for all MTP harms. Initiate progressive sports instruction after three to six weeks as tolerated, and monitor for a recurrence of symptoms. Surgery is warranted only in the most extreme injuries with joint dislocation or harm to the sesamoid bones.
Morton's Neuroma
More common in women than men, Morton's neuroma is a nerve entrapment disease of the nerve between the toes. The nerve becomes thick and painful because of chronic friction together with the adjacent ligaments, for example happens when pivoting in tennis or dancing. Abnormal foot body is thought to contribute to the problem. Athletes whine of burning pain between the feet, at the metatarsal heads.
The pain can improve with rest and worsen with activity. A clinical diagnosis can be made with the lateral squeeze evaluation (see Figure 4).
Since not a true neuroma, but instead a result of entrapment or compression, sneakers with a large toe box generally improve symptoms. Conservative physiotherapy modalities are sometimes helpful. Therapeutic exercises may also help fortify the foot and reduce strain to the injured nerve. When all else fails, surgical decompression or resection of the nerve eliminates the pain, but results in a level of numbness to the area.
Conclusion
Injuries into the mid and forefoot result in a significant number of lost playing time in all sports. By some reports, sports- related injuries to the toes comprise 2% to 18 percent of all athletic injuries(6). While many of those mid and forefoot accidents occur needlessly, they do so in regions already exposed, due to either a decreased blood supply and also the biomechanics of the foot structure.
To minimize these injuries, use orthotics, taping, and therapeutic exercise to correct biomechanical and structural abnormalities inside the foot. Guide your athletes at proper shoe selection, eschewing whatever the shoe business rep could possibly be telling them is so popular. Look closely at functional deficits in gait and regions of relative weakness or strength imbalance. 1 weak gluteus medius muscle sends ripples down the biomechanical string that could leave a participant pivoting on a foot under more pressure than necessary.
References
1. Am Fam Physician. 2003 Jan 1;67(1):85-91.
2. BMJ. 2013 July;3,347:f4561.
3. Clin Sports Med. 1997 July;16(3):435-65.
4. Am Fam Physician. 1999 May 1;59(9):2516-22.
5. Curr Sports Med Rep. Sept/Oct 2011;10(5):249-55.
6. Sports Health. 2012 Nov;4(6):518-34.



 Your new post is loading...
Your new post is loading...









Injury specialist, Dr. Alexander Jimenez reviews the middle and forefoot anatomy -- also discusses several common athletic injuries. For Answers to any questions you may have please call Dr. Jimenez at 915-850-0900